1. Classification by User Capacity (Most Common Clinical Distinction)
This is the primary way medical facilities categorize oxygen chambers, as it directly impacts treatment logistics and patient care.
a. Monoplace Oxygen Chambers (Single-Person Chambers)
- Design & Structure: Compact, sealed units (typically 2–3 meters long, 1 meter in diameter) made of transparent acrylic or steel. They operate as a “closed system”—the entire chamber is filled with 100% oxygen under pressure.
- Pressure Range: 1.5–3 atmospheres absolute (ATA), matching the hyperbaric range required for evidence-based treatments.
- Oxygen Delivery: Patients breathe the 100% oxygen-filled air inside the chamber (no mask needed), simplifying use for those with limited mobility (e.g., patients with non-healing wounds).
- Use Scenarios:
-
- Outpatient treatments (e.g., diabetic foot ulcers, mild CO poisoning).
-
- Emergency care for single patients (e.g., decompression sickness in solo divers).
- Pros: Easy to sanitize, low operational cost, no need for medical staff to enter during treatment.
- Cons: Limited to one patient at a time; narrow space may cause claustrophobia in some users.
b. Multiplace Oxygen Chambers (Multi-Person Chambers)
- Design & Structure: Large, steel-walled chambers (often 4–6 meters long, 2–3 meters in diameter) that can accommodate 2–10 people (patients + 1–2 medical staff). Unlike monoplace chambers, the chamber itself is filled with compressed air (not pure oxygen) to reduce fire risks.
- Pressure Range: 1.5–3 ATA (same hyperbaric range as monoplace).
- Oxygen Delivery: Patients receive 100% oxygen via face masks, hoods, or endotracheal tubes (for intubated patients), while staff breathe compressed air or supplemental oxygen.
- Use Scenarios:
-
- Complex cases requiring in-chamber medical monitoring (e.g., severe necrotizing fasciitis, patients on life support).
-
- Group treatments (e.g., multiple divers with decompression sickness, or radiation injury patients needing regular sessions).
- Pros: Allows hands-on care (e.g., adjusting IVs, monitoring vital signs); reduces claustrophobia with shared space.
- Cons: High installation and operational costs; requires specialized staff to manage pressure and oxygen delivery.
2. Classification by Pressure Level (Hyperbaric vs. Normobaric)
This distinction separates chambers based on whether they exceed atmospheric pressure— a key factor in their therapeutic effects.
a. Hyperbaric Oxygen Chambers (HBO Chambers)
- Definition: Chambers that operate at above 1 atmosphere (ATA) (typically 1.5–3 ATA). This is the only type proven effective for the conditions discussed earlier (DCS, CO poisoning, non-healing wounds).
- Subtypes: Includes both monoplace and multiplace chambers (as above). They are regulated as medical devices (e.g., FDA Class III devices in the U.S.) and require prescription.
- Key Feature: Increases plasma oxygen levels 10–20x compared to normal air, enabling oxygen delivery to oxygen-deprived tissues (e.g., damaged limbs, poisoned brains).
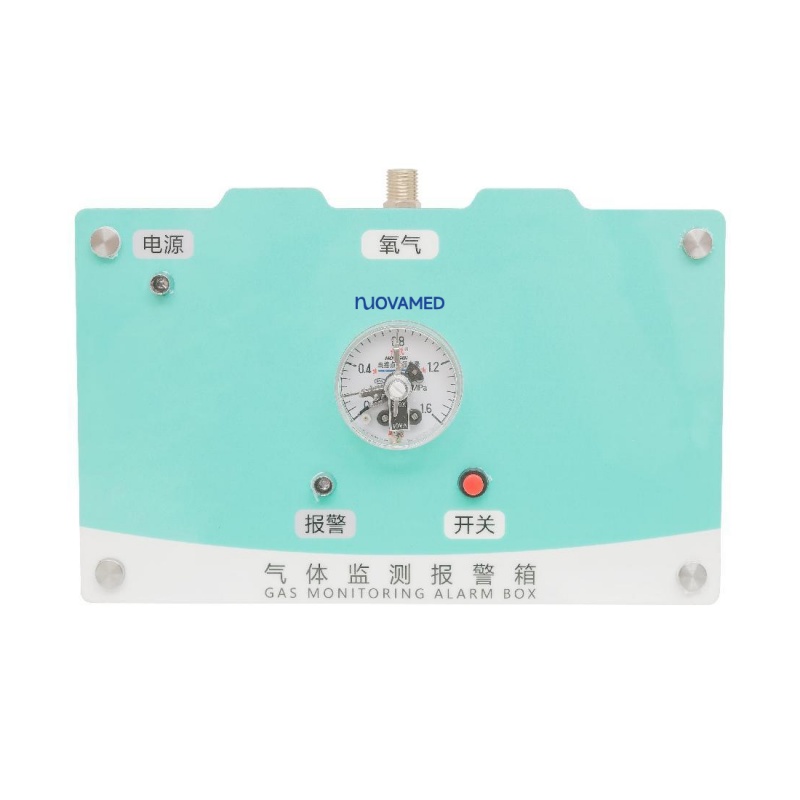
b. Normobaric Oxygen Chambers (Normal-Pressure Chambers)
- Definition: Chambers that operate at 1 atmosphere (ATA) (same as sea-level pressure). They deliver high-concentration oxygen (60–100%) but without increased pressure.
- Design & Types:
-
- Oxygen Tents: Small, tent-like enclosures (for beds) used in hospitals to treat mild hypoxemia (e.g., pneumonia, post-surgery recovery).
-
- Portable Normobaric Chambers: Compact, foldable units (often used at home) that deliver oxygen via a nasal cannula or mask.
- Use Scenarios:
-
- Supporting oxygen levels in patients with mild respiratory issues (not for hyperbaric-indicated conditions).
-
- Some unproven “wellness” uses (e.g., sports recovery), though evidence for these is weak.
- Critical Note: Normobaric chambers cannot replace hyperbaric chambers for conditions requiring increased pressure (e.g., DCS, severe CO poisoning)—their oxygen delivery is no more effective than standard oxygen masks.
3. Specialized Types (Non-Standard Clinical or Industrial Use)
a. Portable Hyperbaric Chambers (Low-Pressure)
- Design: Lightweight, inflatable units (made of durable fabric) that operate at 1.3–1.5 ATA (lower than full clinical hyperbaric levels).
- Use: Emergency on-site treatment (e.g., divers in remote locations, sports injuries) before transfer to a full medical facility.
- Limitation: Not approved for long-term or complex conditions (e.g., non-healing wounds).
b. Industrial Oxygen Chambers
- Purpose: Used in high-pressure work environments (e.g., deep-sea construction) to prevent decompression sickness in workers.
- Design: Similar to multiplace clinical chambers but optimized for industrial teams (e.g., larger space, rugged materials).
Key Comparison of Major Types
|
Feature
|
Monoplace Hyperbaric
|
Multiplace Hyperbaric
|
Normobaric
|
|
Pressure
|
1.5–3 ATA
|
1.5–3 ATA
|
1 ATA
|
|
Oxygen Source
|
Chamber air (100%)
|
Masks/hoods (100%)
|
Masks/tents (60–100%)
|
|
User Capacity
|
1 person
|
2–10 people
|
1–2 people
|
|
Clinical Efficacy
|
Proven for HBO-indicated conditions
|
Proven for HBO-indicated conditions
|
Limited to mild hypoxemia
|
|
Cost
|
Lower
|
Higher
|
Lowest
|
Conclusion
The type of oxygen chamber used depends on treatment goals, patient needs, and clinical guidelines:
- For evidence-based hyperbaric therapies (e.g., DCS, CO poisoning), only monoplace or multiplace hyperbaric chambers (1.5–3 ATA) are effective.
- Normobaric chambers are reserved for mild respiratory support and have no role in hyperbaric-indicated conditions.
- Portable or industrial chambers serve niche emergency or work-related purposes but cannot replace full clinical hyperbaric care.
When considering treatment, always confirm that the chamber meets medical regulatory standards (e.g., UHMS certification) and is prescribed by a hyperbaric medicine specialist.